Have you ever experienced a nagging pain in your lower abdomen, accompanied by an upset stomach? It could be diverticulitis, a digestive disorder that can cause discomfort and disrupt your daily routine. While not everyone with diverticula (small pouches) in their colon experiences inflammation (diverticulitis), it’s important to understand this condition. This article delves into diverticulitis, exploring its causes, symptoms, treatment options, and preventative measures.
The Pouch Party: What is Diverticulosis?
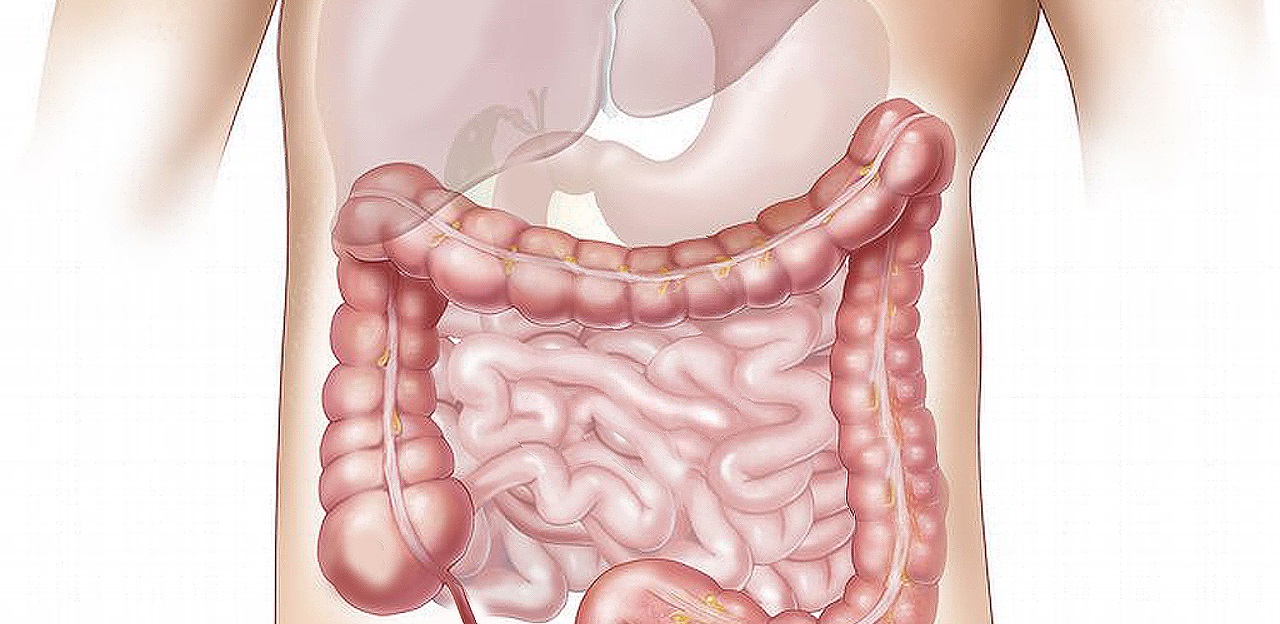
Imagine your large intestine, also known as the colon, as a long, muscular tube responsible for absorbing water and electrolytes from digested food waste. In diverticular disease, pouches develop on the inner lining of the colon. These outpouchings, called diverticula, form when weak spots in the colon wall bulge outward due to pressure.
Diverticulosis, the presence of these pouches, is quite common, especially as we age. In fact, by the age of 80, nearly half of adults in Western countries will have diverticulosis [1]. However, most people with diverticula experience no symptoms and live normal lives.
From Pouch to Ouch: When Diverticula Get Angry (Diverticulitis)
While diverticula themselves are usually harmless, problems arise when they become inflamed or infected. This condition, known as diverticulitis, can be quite painful.
So, what triggers this inflammation?
The exact cause is unknown, but dietary factors are believed to play a role. A low-fiber diet can lead to constipation, which puts increased pressure on the colon walls and may contribute to the formation and inflammation of diverticula.
Here’s a possible scenario: Small, undigested food particles get trapped within the diverticula. This can irritate the colon lining, leading to inflammation and infection.
Painful Reminders: Symptoms of Diverticulitis
Diverticulitis often announces its presence with a sharp, cramping pain in the lower left abdomen, although the location may vary. This pain can be constant or come and go. Here are some other potential symptoms:
- Tenderness in the abdomen, especially when touched
- Fever and chills
- Nausea and vomiting
- Change in bowel habits, such as constipation, diarrhea, or bloody stools
- Difficulty passing gas
Uh Oh, Diverticulitis? What to Do
If you experience these symptoms, seeking medical attention is crucial. Early diagnosis and treatment can help prevent complications. Your doctor will likely perform a physical exam and may order tests like blood tests, a CT scan, or an ultrasound to confirm a diverticulitis diagnosis.
Taming the Angry Pouches: Treatment Options
The treatment approach for diverticulitis depends on the severity of the condition. Here’s a breakdown of possible treatment options:
- Mild Diverticulitis: In most cases, mild diverticulitis can be managed at home with:
- Clear liquids or a low-residue diet for a few days, followed by a gradual reintroduction of solid foods high in fiber.
- Antibiotics to fight infection, if present.
- Pain relievers to manage discomfort.
- Plenty of rest.
- Moderate Diverticulitis: For moderate cases, hospitalization may be necessary for intravenous fluids, antibiotics, and pain management.
- Severe Diverticulitis: In severe cases with complications like abscesses or perforation (a tear in the colon wall), surgery might be needed to remove the inflamed section of the colon or repair the tear.
Preventing the Pain: Keeping Diverticulitis at Bay
While there’s no guaranteed way to prevent diverticulitis, certain lifestyle changes can significantly reduce your risk:
- Fiber Up: A high-fiber diet is key. Aim for 25-35 grams of fiber daily by incorporating fruits, vegetables, and whole grains into your meals. Fiber helps keep your digestive system moving smoothly and reduces pressure in the colon.
- Drink Up: Staying hydrated keeps your digestive system functioning optimally. Aim for eight glasses of water daily.
- Exercise Regularly: Physical activity keeps your digestive system regular and helps maintain a healthy weight.
- Listen to Your Body: Pay attention to your body’s signals. If you experience constipation, address it promptly with dietary changes or laxatives under a doctor’s guidance.
Beyond the Basics: Additional Considerations
Living with diverticulitis requires ongoing management. Here are some additional points to consider:
- Probiotics: Some studies suggest that probiotics, which are live bacteria beneficial for gut health, might help prevent recurrent diverticulitis. However, more research is needed. Discuss this option with your doctor.
- Smoking Cessation: Smoking is a risk factor for diverticulitis. Quitting smoking can significantly improve your overall.
Coping with Diverticulitis Flare-Ups
Even with preventative measures, diverticulitis flare-ups can occur. Here are tips to manage them:
- Rest and Relaxation: Listen to your body and prioritize rest during a flare-up.
- Dietary Adjustments: Switch to a clear liquid or low-residue diet for a few days to allow your colon to rest. Gradually reintroduce high-fiber foods as tolerated.
- Hydration: Staying hydrated is crucial to prevent constipation and promote healing.
- Pain Management: Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage discomfort. Consult your doctor for stronger pain medication if needed.
- Heat Therapy: Applying a heating pad to your abdomen can provide localized pain relief.
When to Seek Medical Attention During a Flare-Up
While some flare-ups can be managed at home, seek immediate medical attention if you experience:
- Severe abdominal pain that doesn’t improve with rest or medication
- Fever and chills
- Bloody stools
- Difficulty passing gas
- Nausea and vomiting that prevent you from keeping fluids down
These symptoms could indicate complications like abscesses or perforation, requiring prompt medical intervention.
Diet and Diverticulitis: A Delicate Balance
Food plays a crucial role in managing diverticulitis. Here are some dietary tips:
- Increase Fiber Intake: Aim for a high-fiber diet, incorporating fruits, vegetables, and whole grains. Fiber helps soften stool and promotes regular bowel movements, reducing pressure on the colon.
- Focus on Soluble Fiber: Soluble fiber, found in fruits, oats, and psyllium husk, forms a gel-like substance in your gut, aiding smooth digestion.
- Limit Red Meat: While not entirely forbidden, excessive red meat consumption may increase inflammation. Opt for lean protein sources like fish, poultry, and legumes.
- Beware of Nuts and Seeds: While healthy overall, nuts and seeds can be difficult to digest and irritate diverticula. Consume them in moderation and choose finely ground options if tolerated.
- Stay Hydrated: Drink plenty of water throughout the day to keep your digestive system functioning optimally.
Living a Full Life with Diverticulitis
Diverticulitis doesn’t have to limit your life. By understanding the condition, making lifestyle changes, and working closely with your doctor, you can manage it effectively. Here are some additional tips for living well with diverticulitis:
- Stress Management: Chronic stress can worsen digestive issues. Practice stress-reduction techniques like yoga, meditation, or deep breathing exercises.
- Regular Doctor Visits: Schedule regular checkups with your doctor to monitor your condition and discuss any concerns.
- Open Communication: Maintain open communication with your doctor. Don’t hesitate to ask questions or express any worries you may have.
Remember: Diverticulitis is a manageable condition. By adopting a proactive approach and working with your healthcare team, you can minimize flare-ups and live a healthy, fulfilling life.
This article provides general information only and does not constitute medical advice. Please consult with your doctor for personalized recommendations regarding diagnosis, treatment, and management of diverticulitis.